All You Should Know About Glaucoma: Risk Factors and Testing!
If it is diagnosed soon, glaucoma can be taken care of to avoid greater decline in eyesight or sight loss. Although, because they are experienced in a gradual manner, the indications of glaucoma can be hard to spot without a test carried out by an eye doctor. If glaucoma hits a late phase without being diagnosed, it may cause severe vision loss.
Glaucoma results from damage to the optic nerve, caused by a boost of fluid pressure in the eye or a problem in the optic nerve itself.
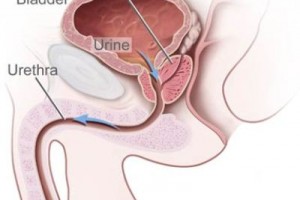
The eye requires a specific amount of pressure to permit the eye to maintain its shape, because it is made up of liquid, called aqueous humour. In a strong eye, this liquid moves throughout the eyeball at a consistent pace. If the drainage tubes which carry the liquid away from the eyeball become clogged, strain starts to develop within the eye. This increase in pressure can cause harm to the optic nerve.
Specific characteristics make an individual more disposed to having glaucoma:
– The main consideration is age. The older someone becomes, the greater the chance of glaucoma developing.
– Someone suffering from short-sightedness or myopia also has a greater chance to develop glaucoma.
– Another significant factor is one’s family history in identifying those people who can be at risk for glaucoma. If you have a family member with glaucoma, your chances of developing the condition are considerably greater.
– Ethnicity is another factor that can have an affect on both an individual’s likelihood of developing glaucoma and the variety of glaucoma. Those of Asian descent are prone to “closed angle” glaucoma, while those of African or Afro-Caribbean nationality are prone to “open angle” glaucoma.
There are six tests that can be given to identify glaucoma. It is strongly urged that anyone over 40 is tested for glaucoma minimally every two years.
Ophthalmoscopy:
For this exam the optometrist inserts eye drops to the eye ball to dilate the pupil. The color and shape of the optic nerve can then be examined. The test is given using a magnifying glass light, which will light up the rear of the eye, making it more clear to see the optic nerve. The optometrist may make use of a digital camera to set aside a photograph of the optic nerve.
Gonioscopy:
The eye will be numbed with eye drops and a mirrored lens is placed alongside the eye to analyze the angle among the iris and the cornea. This is the area of the eye where liquid drains away. The angle between the iris and the cornea tells the optometrist whether the person has “open angle” or “closed angle” glaucoma. The onset of “closed angle” glaucoma is often quite painful, while “open angle” glaucoma forms more gradually and is often much more advanced before a person pays attention to any of the warning signs.
Tonometry:
A very specific tool is used to puff air into the eye, permitting the optometrist to assess the eye pressure. Greater eye pressure is a significant sign of the presence of glaucoma.
Pachymetry:
This test uses a specific device to measure the width of the cornea. By measuring the width of the cornea, an optometrist can better interpret the result of the tonometry test.
Visual Field Testing (Perimetry):
While the individual being examined stares straight ahead, the optometrist brings out little vivid lights at the edge of the person’s peripheral vision. If the patient has difficulty seeing some of the vivid lights, it may indicate that glaucoma has begun to affect his or her vision. This test is usually administered by a computer.



0 Comments
You can be the first one to leave a comment.