Home » Uncategorized »
What Causes Diverticulosis?
What causes diverticulosis? This is a question a patient or family member might ask. As they ask this question they generally have a few ideas of their own. Their preconceived ideas may range from genetic predispositions to consequences of prior injuries or prior GI issues…and to lifestyle and dietary habits. The answer to this question is believed to be in the realm of the later concept; lifestyle factors as they relate to digestive health. This answer is not always welcomed since it implies that the patient “did this to themselves”, but this is not necessarily the idea they should acquire.
There are many aspects in everyone’s life that affect their nutritional choices. For some people their careers or jobs can play a role. For others, complicated prior medical histories might have encouraged the development of diverticula. As we will cover momentarily, a person’s general hydration status can be a factor, and for some jobs and professions it may be difficult to stay adequately hydrated. Also, maintaining a good “mind-bowel” connection is important. It may be difficult for those in some professions to have the freedom to answer “when nature calls” them to have a bowel movement. Not answering this call chronically can weaken a person’s mind-bowel connection…and encourage constipation.
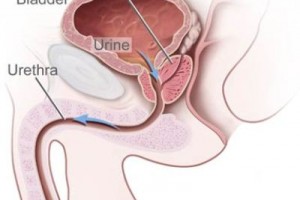
Constipation, especially chronic, is believed to play a large role in developing diverticulosis. Why? The answer requires a brief review of a few aspects of the human colon. Diverticula are most commonly found in the narrower portion of the colon. In fairly simple terms, the last part of the colon before the rectum and anus is called the Sigmoid Colon, and this part of the colon generally has a smaller diameter than the preceding parts of the colon. This is similar to a water hose in that a thinner hose will have more resistance to the flow of water. If you connect a large water hose to a thin hose, the flow of water will change and less water will come out of the end of the thin hose because of the resistance to the flow of water presented by the thin hose. Since the sigmoid colon is more narrow, it can be more affected by higher colon pressures.
Constipation can increase what is referred to as intraluminal pressure. As with a water hose, when pressure increases, weak spots in the hose become apparent, but in the case of the colon, the pressure may push the lining of the colon through the wall of the colon and form the sack-like diverticula. The sigmoid section, being narrowest, may fall prey to this pressure more easily.
So the obvious conclusion is that we all need to try to prevent constipation. How can we prevent constipation? One answer almost everyone has for this question is to increase fiber intake. Well, that might help, but there are a few more things to consider. As mentioned earlier, a person should not ignore their need to use the rest room for a bowel movement; when nature calls we need to listen. The other big and often under-appreciated aspect in bowel regularity is hydration status. Simply dumping more fiber into a colon won’t necessarily correct constipation if there isn’t enough water available to mix with the fiber, soften the stool, and encourage the movement of the stool through the colon. Without adequate hydration, the added fiber can actually encourage constipation, bloating, cramping, and unpleasant gas. Even when a person is great about ensuring good hydration, they should increase total fiber intake slowly over the course of a few weeks to allow their digestive system to adapt to the change. Otherwise, they may still experience the digestive issues just noted and be tempted to revert back to a lower fiber intake.
Although, nutritional changes and lifestyle changes may significantly reduce your chances of developing troublesome diverticulosis, medications can affect digestive system functioning and should not be overlooked. Use of prescription pain medications and muscle relaxers can cause constipation and altered bowel movements. Medications called motility agents may help, but a visit with your primary care provider to discuss such medications is the best way to find out if this is necessary. Also, a history of using antibiotics that have caused diarrhea can lead to altered levels of good bacteria in the gut, which over time can encourage chronic constipation is some people.
If preexisting health conditions exist that affect the digestive system, such as diabetic gastroparesis seen in people with a history of poorly controlled diabetes mellitus, a person’s primary doctor must be involved in treating constipation and medications may be required. For an otherwise healthy individual, healthy nutrition and lifestyle changes may be all that’s needed to maintain bowel regularity and decrease the risk of diverticulosis. Good and balanced nutrition and, when appropriate, supplementation, can play a huge role in the prevention, management and treatment of many gastrointestinal condition, especially conditions directly tied to nutrition and lifestyle like diverticulosis and diverticulitis. Supplements such as prebiotics and probiotics, fiber blends, and fish oil can help to reduce a person’s risk of a whole host of health conditions. When speaking about prevention of diverticulosis, and many other health conditions, the emphasis is on minimizing risk factors that are known to play a role in the development.
As with many things in life, the development of diverticulosis is not always predictable or fair. One person may be physically active, eat a well-balanced diet, and maintain appropriate hydration…yet still develop diverticulosis. Nevertheless, the overall risk of developing diverticulosis is something we can mitigate.
Low risk does not imply “no risk.” The chances of winning the lottery are extremely low, but people still win. Also, it should be noted that having diverticulosis, meaning that diverticula are present in the colon, may not pose any health risk for some people, but others may develop infections of the diverticula leading to the painful condition called diverticulitis. Obviously, preventing the formation of diverticula all together is the best way to avoid the infection, pain, and bleeding associated with diverticulitis.
Limited physical activity should also be part of this list of contributing factors because being inactive can encourage constipation. Being active, on the other hand, encourages better functioning of the digestive system as it relates to bowel regularity. Age is a risk factor as well, but unfortunately it’s something out of our control. As we age the muscle tone of the colon may weaken, therefore advanced age may increase a person’s risk of developing diverticula. In fact, more than 25% of people over the age of 55 will have at least one diverticulum.
In summary, the primary suspected cause of developing diverticulosis is elevated intraluminal pressure, which can be a result of constipation and irregular or delayed bowel movements. Various lifestyle factors that are known to encourage constipation are agonists in the development of diverticulosis; diets low in fiber, less than optimum hydration status, advanced age, ignoring the mind-bowel signal to have a bowel movement, and being physically inactive. Anything that leads to constipation also directly increases the chances of diverticula creation.